- Overview
- BIN-PCN for Routing Supplemental Transactions
- Part D Plans
- - Nx Reject Reports
- - Annual Report Distribution Email Setup and Changes after Annual Submission
- - Nx Realtime
- - Nx Update Process
- - Nx Replay Request
- - Nx History Request
- - FAQ
- - Nx Implementation and Testing
- - Business Associate Agreement (BAA)
- Supplemental Payers
As part of the CMS Coordination of benefits requirement, a sponsor must have processes in place to appropriately respond to transactions that provide supplemental coverage information (N transactions).
Some Sponsor's processors/PBMs have the ability to replay Nx transactions within their systems when readjudication or system corrections are made. As such, sponsors need the ability to report a status change for an Nx transaction previously transmitted by the transaction facilitator.
This page contains information on the process behind updating the status of an Nx transaction previously transmitted by the transaction facilitator.
Plans may submit updated transaction status information via the standard Nx Status Update Request file, which can be found in the Related Documents section of this page. The transaction facilitator will return a file with information pertaining to the results of the update request. The process flow is as follows:
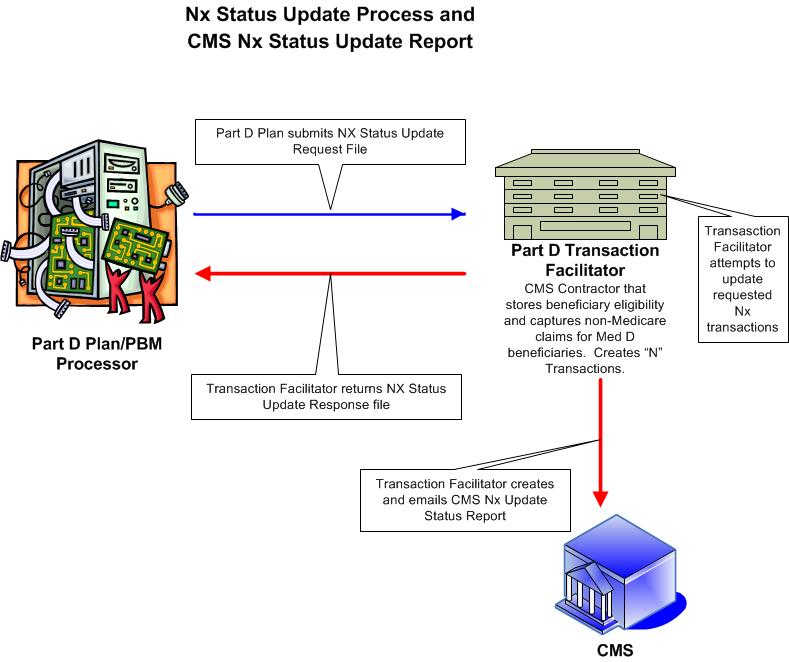
This flowchart depicts the flow of how plans can update status of an N transaction(s) previously processed. The plan can send a file to the Transaction Facilitator with the updated status of a transaction. The Transaction Facilitator will process the file and if applicable, update the status of the transaction. This in turn updates N transaction reports for both the plan and for CMS.
The Nx Status Update Process and Report Guide provides file specification, process information and scenarios.
All Nx Status update requests should be submitted to TBTSupport@relayhealth.com