Hospice providers and Medicare Part D sponsors identified the need for a standardized form to facilitate communication regarding a beneficiary’s hospice election status between all involved parties. Although an optional form was approved for use by the Office of Management and Budget (OMB), the process is cumbersome and found to be largely ineffective, as the hospice provider may not be aware of the beneficiary’s enrollment in Medicare Part D. This information is currently faxed from hospice to the pharmacy/Medicare Part D sponsor. Furthermore, the current method does not support The Center for Medicare and Medicaid Services’ (CMS) desire to achieve interoperability and standardized information sharing with covered entities, it is the best solution available at this time.
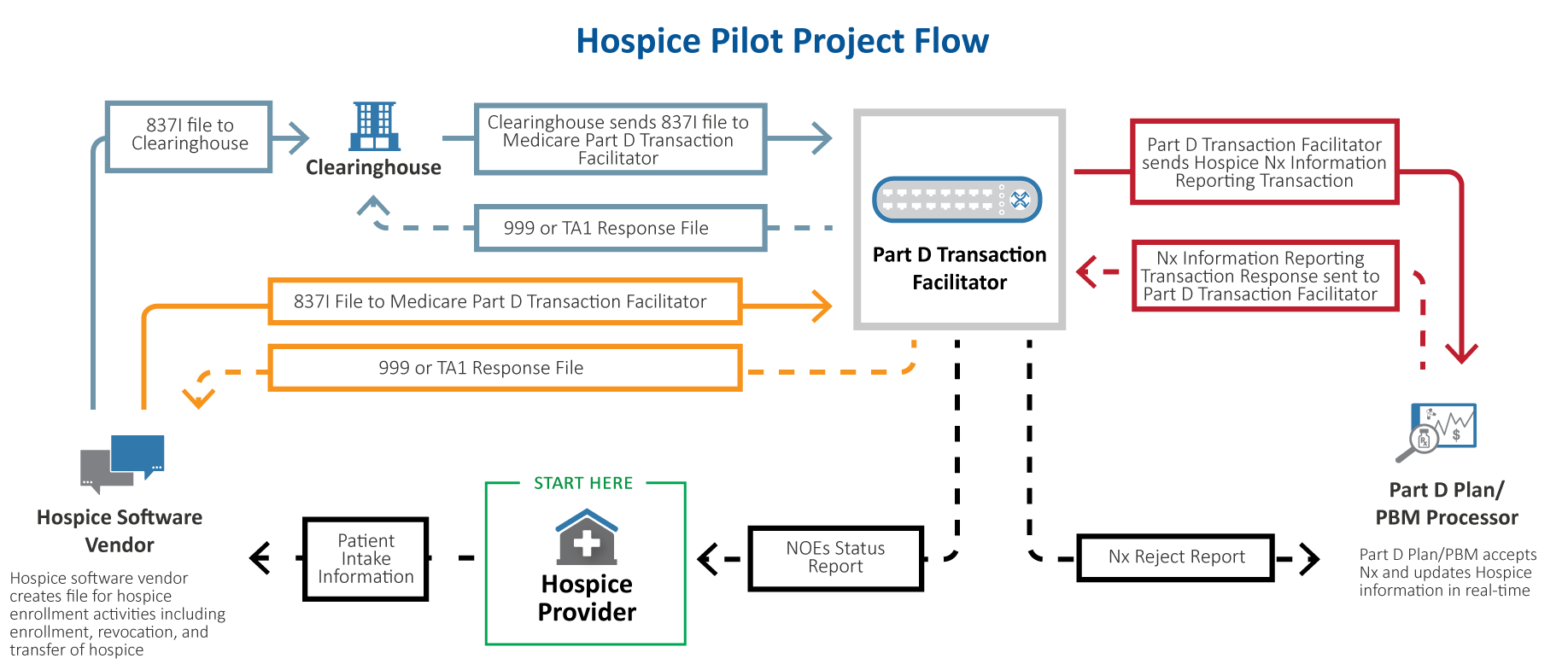
To resolve the issues identified above, the industry has created a pilot program that shortens the hospice election status notification timeframe. CMS has contracted with the Medicare Part D Transaction Facilitator (RelayHealth) to design a hospice election notification system. The Medicare Part D Transaction Facilitator is working with national hospice stakeholder organizations, NCPDP WG9 Hospice Task Group and other industry stakeholders on the development of the pilot program. This pilot will provide the notice of hospice election to the Medicare Part D sponsors in a timely manner. Medicare Part D sponsors will be able to utilize hospice election status for purposes of drug coverage determinations, with the intent of minimizing latent subrogations.
This Hospice pilot will be rolled out in two phases and is designed to replace the form with an electronic automated notification:
Phase One: The hospice election notification will be automated using a copy of existing Health Insurance Portability and Accountability Act of 1996 (HIPAA) 837I electronic transaction, allowing the Medicare Part D sponsors to put edits in place for coordination of benefits and to mitigate erroneous payment for hospice related medications paid under the Part D benefit.
Hospice providers participating in this “end-to-end” pilot will receive a report that provides:
- Identification of beneficiaries for which the Medicare Beneficiary Identifier (MBI) cannot be matched.
- Identification of beneficiaries not enrolled in Medicare Part D.
- Identification of the beneficiary’s Medicare Part D sponsor.
- Acknowledgement of successful acceptance or rejection by the beneficiary’s Medicare Part D sponsor.
Note: Medicare Part D eligibility will be continuously reassessed to provide updated notification in the event of a Medicare Part D sponsor enrollment change.
Medicare Part D sponsors participating in this “end-to-end” pilot will receive notification that their beneficiary is in hospice.
Phase Two (to be launched at a future date): Covered medication lists will be sent to the Medicare Part D sponsors:
- Hospice Providers will transmit covered medication information to the Medicare Part D Transaction Facilitator (RelayHealth).
- Medicare Part D Transaction Facilitator will transmit covered medication information to the beneficiary’s Medicare Part D sponsor.
- Medicare Part D sponsor will be able to put edits in place to recognize which medications are not covered by hospice.