As discussed in the Supplemental Payer Overview Section, there are multiple steps to ensure that record of a supplemental payment can be transmitted to the Part D Plan.
Because CMS does not regulate Supplemental Payers, it cannot require supplemental plans to only pay claims when the 4Rx (BIN/PCN/Group and Cardholder ID) on the claim matches the 4Rx sent to CMS on the Supplemental Payers eligibility file.
However, for the Transaction Facilitator to match the paid claims to the eligibility record, the 4Rx must match. If the Supplemental Payer chooses to allow claims submitted by a pharmacy to have different 4Rx, an alternative batch file submission can be utilized to ensure that the 4Rx matches.
In this situation, when the Supplemental Payer creates the batch file, the 4Rx that was submitted on the claim would be overlaid in the batch file with the 4Rx that is submitted to CMS. This ensures that the Transaction Facilitator can find a supplemental eligibility match and forward the Transaction to the Part D Plan.
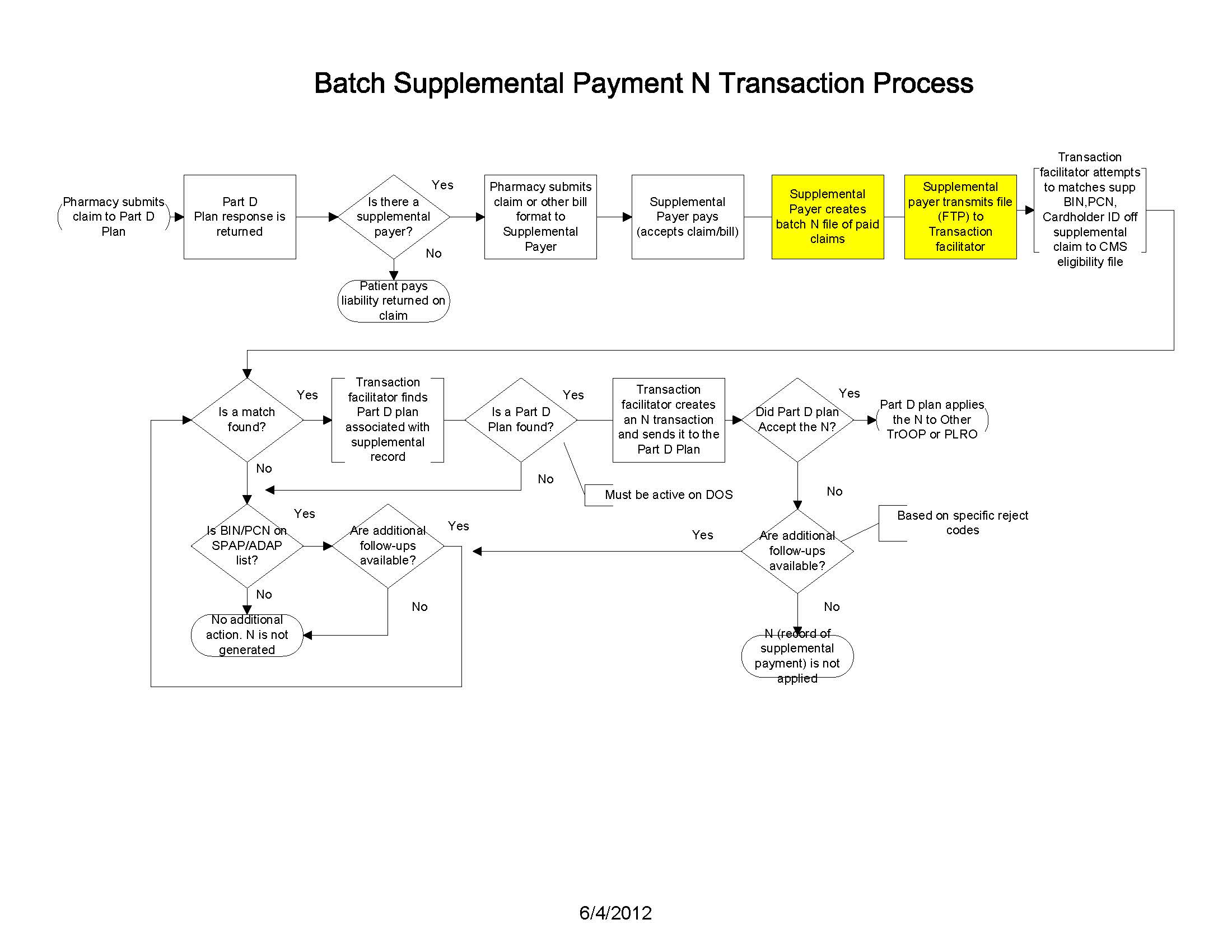
If a Supplemental Payer chooses to submit a batch file to the Transaction Facilitator it will need to notify the Transaction Facilitator to use the batch files submitted by the Supplemental Payer and not to use real-time transactions from the switches.
Additionally, there are other reasons that may require the use of the batch file format. If the Supplemental Payer:
- allows beneficiaries to submit paper claims. Paper claims are paid directly by the Supplemental Payer without pharmacy or switch involvement, therefore the only available method for communicating payment of paper claims is via the batch Nx file process.
- has a direct connection to a pharmacy. In this situation, the pharmacy does not use a switch to submit claims to the Supplemental Payer.
- does not process claims in real-time or batch, and does not have a processor that performs these functions.
- has adjusted the original supplemental claim (impacting the supplemental copay) through an offline process. (not through electronic pharmacy transaction). In this situation, the Supplemental Payer needs to provide updated supplemental copay information to the Part D Plan.
The batch file specifications are contained in Batch Supplemental Information Reporting (N Transaction) which can be found in the Nx Supplemental Payer Sheets section of this page.
Additionally, if the Supplemental Payer’s processor does not have an FTP set up with the Transaction Facilitator, to ensure secure transfer of claims and PHI information, it will need to complete and follow the FTP setup instructions in the RelayHealth Batch File FTP for Supplemental N Transaction Form which can be found in the Related Documents section of this page.
In addition to the FTP setup process, for Supplemental Payers new to the Nx Batch submission process, information related to testing process is outlined in Supplemental Plan Batch N File to the Transaction Facilitator Testing Process which can be found in the Related Documents section of this page.